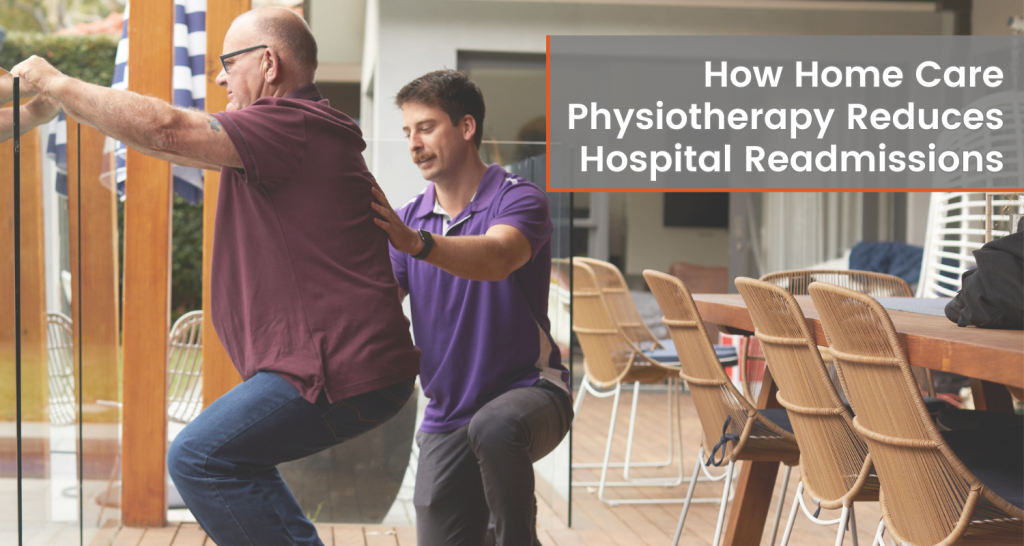
The healthcare landscape has shifted significantly in recent years, with a growing emphasis on innovative, person‑centred solutions that improve outcomes and reduce unnecessary hospital readmissions. One highly effective approach is Physiotherapy delivered in the home, a model of care that brings personalised rehabilitation directly to the person’s doorstep.
This blog explores how home-based Physiotherapy supports recovery, prevents complications, and ultimately reduces the likelihood of hospital readmission.
What Are Hospital Readmissions and Why Do They Happen?
Hospital readmissions occur when a person returns to hospital shortly after being discharged—often within 30 days. These readmissions may result from:
- Complications after surgery or illness
- Limited access to follow‑up care
- Poor mobility or functional decline
- Inadequate support at home
High readmission rates place strain on healthcare systems and often signal that people are not receiving the ongoing care they need to recover safely.
How Home Care Physiotherapy Helps Reduce Readmissions
Home-based Physiotherapy offers a proactive, accessible, and personalised approach to rehabilitation. By delivering expert care directly to the person’s home, Physiotherapists can address barriers that often contribute to readmission.
- Personalised, Goal‑Focused Rehabilitation
Physiotherapy in the home allows clinicians to design tailored treatment plans based on the person’s unique needs, environment, and recovery goals. This personalised approach supports:
- Better engagement in therapy
- Improved adherence to exercises
- Faster functional gains
By working within the person’s actual living environment, Physiotherapists can also recommend practical modifications to enhance safety and independence.
- Greater Convenience and Accessibility
Many people face challenges attending clinic appointments due to:
- Mobility limitations
- Lack of transport
- Fatigue or pain
- Chronic health conditions
Home care Physiotherapy removes these barriers, ensuring consistent treatment. Regular, uninterrupted therapy is a key factor in preventing complications that could lead to hospital readmission.
- Early Detection and Prevention of Complications
In-home Physiotherapists can identify early warning signs such as:
- Declining mobility
- Increased pain
- Respiratory issues
- Falls risk
- Poor wound healing
By intervening early, clinicians can prevent minor issues from escalating into serious problems requiring hospitalisation. This proactive monitoring is one of the strongest advantages of home-based care.
- Education That Empowers the Person and Their Family
Education is a powerful tool in preventing readmissions. During home visits, Physiotherapists can teach:
- Safe mobility and transfer techniques
- Effective exercise routines
- Strategies for managing symptoms
- How to follow medical advice correctly
Empowering people and their families with knowledge promotes confidence, independence, and better long‑term outcomes.
The Broader Impact on Healthcare Systems
Reducing hospital readmissions benefits not only the individual but also the healthcare system. Fewer readmissions mean:
- Lower healthcare costs
- Reduced pressure on hospital beds
- Improved continuity of care
- Better overall population health outcomes
Home care Physiotherapy plays a crucial role in achieving these goals by providing high‑quality, person‑centred rehabilitation where it’s needed most.
Home-based Physiotherapy remains one of the most effective ways to reduce hospital readmissions. With personalised care, improved accessibility, timely intervention, and a strong focus on education, mobile Physiotherapists help people recover safely and confidently in the comfort of their own homes.
As healthcare continues to evolve, Physiotherapy delivered at home will remain a vital part of post‑discharge support—promoting independence, wellbeing, and long‑term health.
For those seeking trusted, high‑quality home care, Empower Healthcare Physio provides comprehensive mobile Physiotherapy services designed to support safer, smoother recoveries.
…